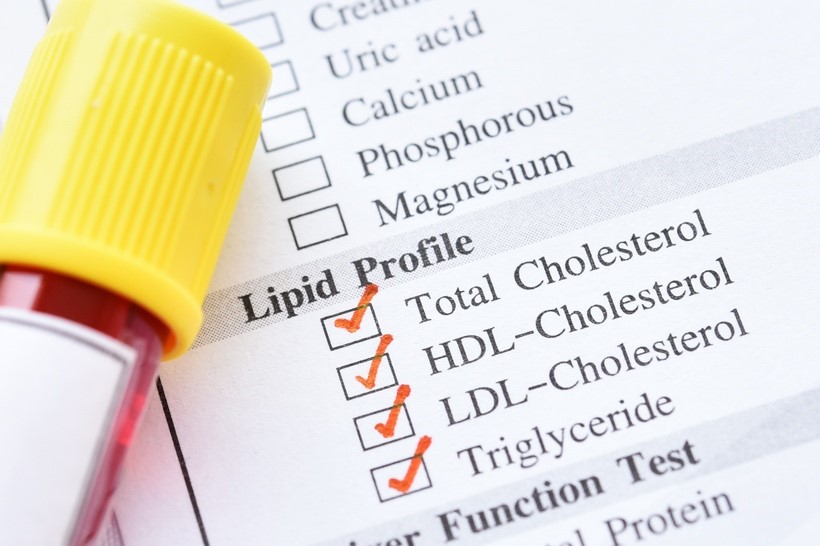
Cholesterol is measured in a lipid panel (also known as a lipid profile), which typically consists of total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and triglycerides (TGs).1,2 High levels of lipids like cholesterol in the blood serum, known as hyperlipidemia, increase the risk of atherosclerotic cardiovascular disease (ASCVD).2 Cholesterol is often used as a biomarker to measure risk of ASCVD conditions. Namely, LDL-C and non-high-density lipoprotein cholesterol (non-HDL-C) are primary indicators of risk of coronary heart disease and primary targets for treatment.2 TC and HDL levels, together, can also be used to determine ASCVD risk.1
TC and HDL-C are directly measured from the blood serum in mg/dL. These values are then used in mathematical equations to estimate LDL-C levels. Traditionally, the Friedewald equation, [LDL-C = TC – HDL-C – (TG/5)], is used. Here, five refers to the 5:1 concentration ratio of fasting triglyceride to very low-density lipoprotein (VLDL), an LDL-C precursor; dividing fasting triglyceride level by five yields thus yields the concentration of VLDL.1,3 However, the accuracy of the Friedewald equation is limited by TG and actual LDL-C levels, where high TG (>200mg/dL) and low LDL-C level yields an underestimation of actual LDL-C. Additionally, the equation underestimates levels of intermediate-density lipoprotein (IDL) and remnant VLDL which may contribute to atherogenesis. As such, direct LDL-C assays may be used in place of the Friedewald equation when these limitations exist. Moreover, the Martin Hopkins Formula has been developed as a complex, but more accurate alternative formula for estimating LDL-C in high TG and low actual LDL-C settings. This formula is present on online calculator platforms, which quickly bypasses its complexity disadvantage. It is currently adopted by major laboratories such as Quest Diagnostics.4
Non-HDL-C and remnant cholesterol can be calculated using the following formulas, respectively: non-HDL-C = TC– HDL-C and remnant cholesterol = TC – LDL-C – HDL-C.4
Historically, patient fasting was a requirement before performing a lipid panel.5,6 However, recent recommendations by organizations such as the National Lipid Association, American Heart Association, and American College of Cardiology support the use of either fasting or non-fasting lipid panels for measuring baseline cholesterol levels and diagnosing ASCVD risk.7,8 Fasting lipid profiles involve an overnight fast of at least 8 hours, with allowed consumption of water, black coffee, and tea without milk, followed by a blood draw for serum TC, HDL-C, TG, and calculated LDL-C levels. 4,9 Support for the traditional method stems from the fact that the triglyceride level increases following food intake, potentially decreasing the accuracy of TG measurement, LDL-C calculation, and the estimated ASCVD risk.6,9 This form of lipid measurement is recommended for patients suspected to have genetic dyslipidemias to allow for a clear identification of the lipid abnormality, as well as for patients with borderline dyslipidemia to accurately determine whether to initiate treatment.9,10 It may also be used when patients have elevated baseline TG levels, are receiving treatment to lower LDL-C, or to follow up on a non-fasting lipid panel where TG levels appear notably high (>400 mg/dL).9 Disadvantages to a fasting lipid panel includes increased risk of hypoglycemia in people with diabetes taking antidiabetic medication, likely due to residual effects of insulin during the fast.11,12 Non-fasting is also more convenient and equally predictive of ASCVD.6,9,10 Fasting before a visit also presents a lifestyle inconvenience for patients.6
Increased convenience may also enhance patient compliance in receiving routine lipid screenings.10 Increased TG levels following food intake often underestimates LDL-C levels when used in Friedewald equation. However, use of the Hopkins Martin formula yields estimated LDL-C values that are more representative of actual LDL-C levels.13 Additionally, recent studies have indicated similarities in ASCVD prognosis for fasting and non-fasting panels, minimizing the significance of postprandial TG elevation.14 Either fasting or non-fasting lipid panels can be used to measure patient cholesterol levels.
Reference
- Stone NJ, Bilek S, Rosenbaum S. Recent National Cholesterol Education Program Adult Treatment Panel III Update: Adjustments and Options. The American Journal of Cardiology. 2005/08/22/ 2005;96(4, Supplement):53-59. doi:https://doi.org/10.1016/j.amjcard.2005.06.006
- Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. May 16 2001;285(19):2486-97.
- Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. Jun 1972;18(6):499-502.
- Pasternak RC. 2001 National Cholesterol Education Program (NCEP) Guidelines on the Detection, Evaluation and Treatment of Elevated Cholesterol in Adults: Adult Treatment Panel III (ATP III). ACC Current Journal Review. 2002/07/01/ 2002;11(4):37-45. doi:https://doi.org/10.1016/S1062-1458(02)00670-0
- Langsted A, Nordestgaard BG. Nonfasting versus fasting lipid profile for cardiovascular risk prediction. Pathology. Feb 2019;51(2):131-141. doi:10.1016/j.pathol.2018.09.062
- Nordestgaard BG. A Test in Context: Lipid Profile, Fasting Versus Nonfasting. J Am Coll Cardiol. Sep 26 2017;70(13):1637-1646. doi:10.1016/j.jacc.2017.08.006
- Jacobson TA, Ito MK, Maki KC, et al. National Lipid Association recommendations for patient-centered management of dyslipidemia: part 1 - executive summary. J Clin Lipidol. Sep-Oct 2014;8(5):473-88. doi:10.1016/j.jacl.2014.07.007
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. Jun 25 2019;73(24):3168-3209. doi:10.1016/j.jacc.2018.11.002
- Rahman F, Blumenthal RS, Jones SR, Martin SS, Gluckman TJ, Whelton SP. Fasting or Non-fasting Lipids for Atherosclerotic Cardiovascular Disease Risk Assessment and Treatment? Curr Atheroscler Rep. Feb 17 2018;20(3):14. doi:10.1007/s11883-018-0713-2
- Naugler C, Sidhu D. Break the fast?: Update on patient preparation for cholesterol testing. Can Fam Physician. 2014:895-7. vol. 10.
- Aldasouqi S, Sheikh A, Klosterman P, et al. Hypoglycemia in patients with diabetes who are fasting for laboratory blood tests: the Cape Girardeau Hypoglycemia En Route Prevention Program. Postgrad Med. Jan 2013;125(1):136-43. doi:10.3810/pgm.2013.01.2629
- Aldasouqi S, Sheikh A, Klosterman P, et al. Hypoglycemia in patients with diabetes on antidiabetic medications who fast for laboratory tests. Diabetes Care. 2011:e52. vol. 5.
- Sajja A, Park J, Sathiyakumar V, et al. Comparison of Methods to Estimate Low-Density Lipoprotein Cholesterol in Patients With High Triglyceride Levels. JAMA Network Open. 2021;4(10):e2128817-e2128817. doi:10.1001/jamanetworkopen.2021.28817
- Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III). Circulation. Aug 12 2014;130(7):546-53. doi:10.1161/circulationaha.114.010001
.png)

