A stroke is a brain injury that occurs when a part of the brain is without blood for too long.1 Strokes can be categorized as ischemic, intracerebral hemorrhage, or subarachnoid hemorrhage. Ischemic strokes occur due to blockages in the blood vessels that supply the brain. Hemorrhagic strokes occur due to a leakage or rupture of the blood vessels that supply the brain. In the United States, 87% of all strokes are ischemic and the remaining 13% are intracerebral or subarachnoid hemorrhagic.2,3
Stroke symptoms frequently have an acute onset. One study (n=176) found that 96% of stroke patients had acute onset of symptoms.4 Symptoms for ischemic stroke and intracerebral hemorrhagic stroke are similar, with the most common symptoms being difficulty speaking and weakness of half of the body.5 A study of 176 patients with stroke or transient ischemic attack (TIA) found the following prevalence of patient reported symptoms: acute onset (96%), arm weakness (63%), leg weakness (54%), speech disturbance (53%), facial weakness (23%), loss of arm sensation (20%), loss of leg sensation (17%), headache (14%), non-orthostatic dizziness (13%).4 The study also found the following prevalence of clinically assessed signs of stroke: facial paresis (45%), arm paresis (69%), leg paresis (61%), visual field defect (24%), eye movement abnormality (27%), dysphasia/dysarthria (57%), visuospatial neglect (23%), hemiparetic/ataxic gait (53%), and arm sensory defects (23%), and leg sensory defects (21%). Reliably distinguishing between intracerebral hemorrhage and ischemic stroke can only be done through neuroimaging.5
Subarachnoid hemorrhagic stroke presents differently than ischemic stroke or intracerebral hemorrhagic stroke.5,6 The most common symptom is described by patients as “the worst headache of my life.” Symptoms may also include vomiting, seizures, headache, neck stiffness, photophobia, and decreased level of consciousness.6
The duration of symptoms directly impacts outcomes. While there are treatments that can help those who have suffered a stroke, most are only effective within the first several hours of onset. Guidelines in the United States, Europe, and Canada recommend endovascular recanalization up to six hours after symptom onset, and the US Food and Drug Administration (FDA) has approved the use of thrombectomy devices up to eight hours after symptom onset.7-9 Thus, it is important to seek help immediately if someone suspects they’re having a stroke.
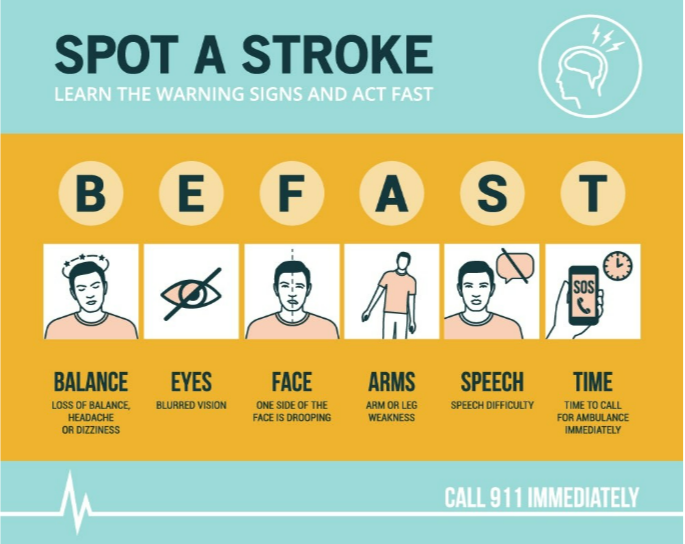
The BE FAST (balance, eyes, face, arms, speech, time) mnemonic device has been developed to help identify acute ischemic stroke.10 B refers to loss of balance, E refers to the eyes having blurred vision, F refers to facial droop or weakness, A refers to arm or leg weakness, S refers to slurred speech, and T refers to the need for immediate, timely treatment of strokes to prevent permanent neurologic deficits.
References
- Caplan L, Caplan's Stroke, p.22-63. Basic pathology, anatomy, and pathophysiology of stroke. Caplan's Stroke: A Clinical Approach. 4 ed. Saunders Elsevier; 2009:22-63.
- Rosamond W, Flegal K, Furie K, al e. Heart disease and stroke statistics–2008 update: a report from the Ameri Statistics Subcommittee. Circulation. 2008;117(4):25-146.
- Adams H, Bendixen B, Kappelle L, Love B, Gordon D, Marsh E. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35-41.
- Nor A, Davis J, Sen B, al e. The Recognition of Stroke in the Emergency Room (ROSIER) scale: development and validation of a stroke recognition instrument. Lancet Neurol 2005;4(11):727-734.
- Yew K, Cheng E. Acute stroke diagnosis. Am Fam Physician. 2009;80(1):33-40.
- Suarez J, Tarr R, Selman W. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006;354(4):387-396.
- Powers W, Rabinstein A, Ackerson T, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2019;50(12):344-418.
- Turc G, Bhogal P, Fischer U, et al. European Stroke Organisation (ESO) - European Society for Minimally Invasive Neurological Therapy (ESMINT) Guidelines on Mechanical Thrombectomy in Acute Ischemic Stroke J Neurointerv Surg. 2019;doi:10.1136/neurintsurg-2018-014569
- Casaubon LK, Boulanger JM, Blacquiere D, et al. Canadian Stroke Best Practice Recommendations: Hyperacute Stroke Care Guidelines, Update 2015. Int J Stroke. Aug 2015;10(6):924-40. doi:10.1111/ijs.12551
- Aroor S, Singh R, Goldstein L. BE-FAST (Balance, Eyes, Face, Arm, Speech, Time): Reducing the Proportion of Strokes Missed Using the FAST Mnemonic. Stroke. 2017;48(2):479–481. doi:10.1161/STROKEAHA.116.015169