Hyperlipidemia or dyslipidemia, colloquially known as high cholesterol, is characterized by high blood serum levels of low-density lipoprotein (LDL) and triglycerides and low levels of high-density lipoprotein (HDL).1 All of these measurements together are known as total cholesterol (TC).
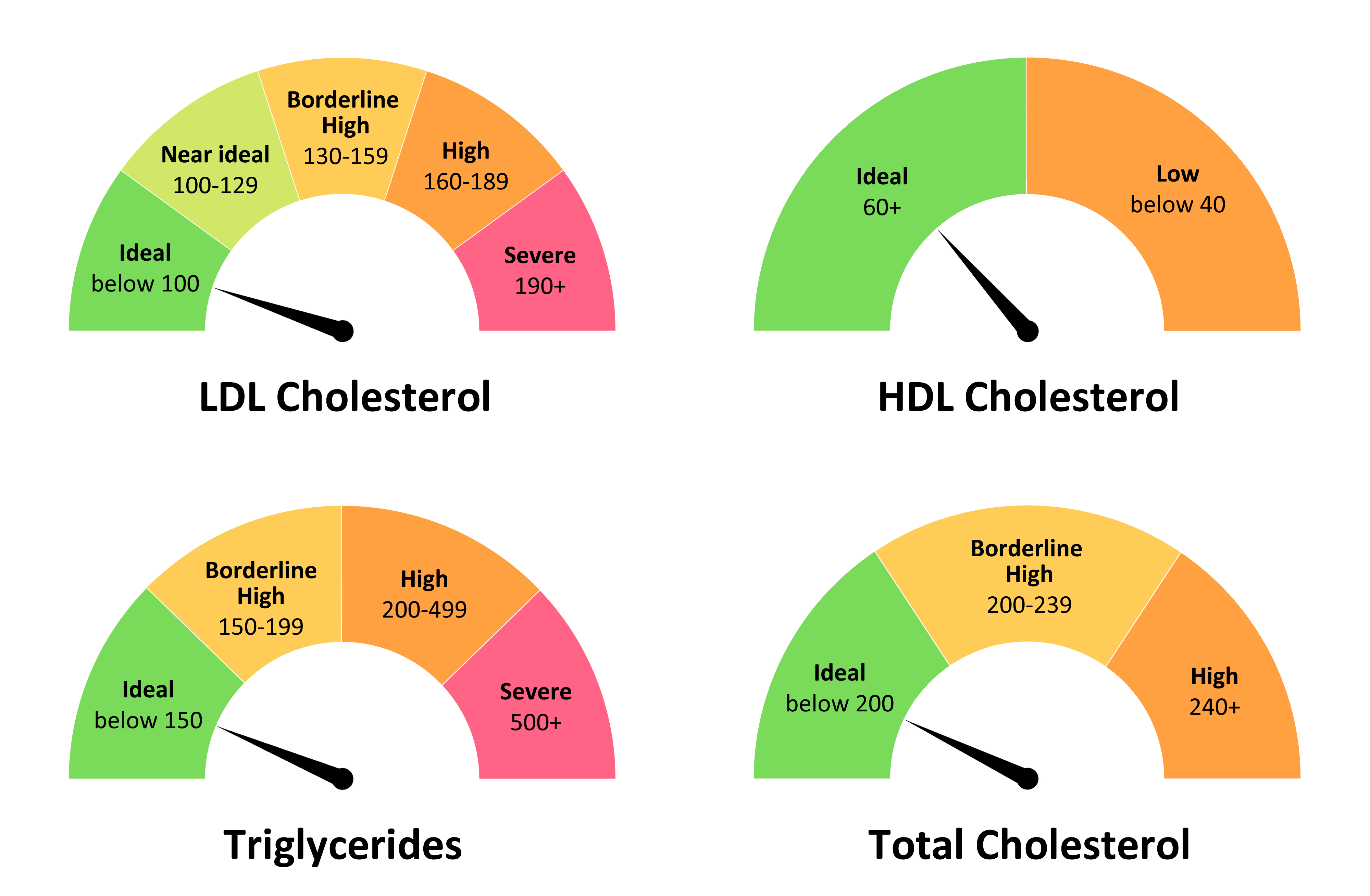
Table 1. Recommended cholesterol levels for otherwise healthy adults presented in mg/dL1,2
|
LDL
|
|
Ideal
|
<100
|
|
Near optimal
|
100-129
|
|
Borderline high
|
130-159
|
|
High
|
160-189
|
|
Severe
|
≥190
|
|
Triglycerides
|
|
Ideal
|
<150
|
|
Borderline high
|
150-199
|
|
High
|
200-499
|
|
Severe
|
≥500
|
|
TC
|
|
Ideal
|
<200
|
|
Borderline high
|
200-239
|
|
High
|
≥240
|
The 2018 American Heart Association/American College of Cardiology (AHA/ACC) Guideline on the Management of Blood Cholesterol focuses on low-density lipid cholesterol (LDL-C) level, existing atherosclerotic cardiovascular disease (ASCVD), as well as 10-year ASCVD risk when making management decisions.3 Severe hypercholesterolemia is defined as a low-density lipid cholesterol (LDL-C) level of ≥190 mg/dL.3,4 The optimal level of LDL-C is <100 mg/dL for most people. However, the guideline sets a threshold of LDL-C of 70 mg/dL for people with existing ASCVD or diabetes or who have a very high 10-year ASCVD risk.3 The overarching message of the guideline that “lower is better” when it comes to LDL-C levels.
Measurement of total cholesterol (TC) and high-density lipoprotein cholesterol (HDL-C) are central to the determination of cardiovascular risk and are used to calculate low-density lipoprotein cholesterol (LDL-C).1,2 LDL-C is the dominant form of atherogenic cholesterol and thus the target of lipid-lowering therapies to lower that risk.2,3 Population studies have shown that the optimal level of LDL-C is about 100 mg/dL.4,5
The 2018 American Heart Association (AHA)/ American College of Cardiology (ACC) clinical practice guidelines for the management of blood cholesterol recommend the following targets of lipid-lowering therapy:2
- In patients with clinical atherosclerotic cardiovascular disease (ASCVD), lower LDL-C levels by 50%
- Use a threshold of 70 mg/dL in very high-risk individuals when considering the addition of non-statins to statin therapy. Very high-risk individuals include those with multiple major ASCVD events or one major ASCVD event and multiple high-risk conditions.
- People with severe hypercholesterolemia (LDL≥190 mg/dL) should consider use of non-statin therapy added to statin therapy to achieve levels below 100 mg/dL.
- People with diabetes (between the ages of 40 and 75 years) should take statins to lower their ASCVD risk. If they have other risks for ASCVD, it is reasonable to lower the LDL-C by 50% using high-intensity statins.
- Adults 40 to 75 years of age without diabetes or clinical ASCVD, with LDL-C levels of 70 mg/dL or higher may benefit by lowering the LDL-C depending on their calculated 10-year risk of ASCVD. If statins are recommended, the targets range from a 30% reduction of LDL-C levels to a 50% reduction.
Although LDL-C remains the therapy target in current guidelines,2 measurement of TC and HDL-C has been shown to be useful in calculating ASCVD risk, most often as a ratio of TC to HDL-C.6 Ingelsson et al. used data from a cohort (n=3322) of the ongoing Framingham Heart Study to determine the clinical value of lipid measurements in predicting coronary heart disease.6 After a median follow-up of 15 years, 291 of the participants developed coronary heart disease. The ratio of TC to HDL-C performed better than individual lipid levels in calculating ASCVD risk. TC and HDL-C levels are often used in the calculation of LDL-C and are reliable whether taken after food or fasting, making them useful measurements for screening tests.2 Ideal total cholesterol is <150 mg/dL and the ideal HDL-C is >60 mg/dL.2
There is insufficient evidence that lowering triglyceride levels improves cardiovascular health.7 The most serious complication of very high triglycerides is the development of pancreatitis. But high levels of triglycerides often accompany visceral adiposity, diabetes, and fatty liver disease. For this reason, elevated triglyceride is considered a biomarker for cardiovascular disease risk. Persistently elevated primary hypertriglyceridemia (≥175 mg/dL) is considered an ASCVD risk-enhancer according to the 2018 AHA/ACC cholesterol guidelines.2 Although these numbers do not yet constitute a therapeutic target, triglyceride levels are defined as follows:7
- Normal <150 mg/dL
- Borderline high 150 to 199 mg/dL
- High 200 to 499 mg/dL
- Very high ≥500 mg/dL
Measurement of apolipoprotein B (apo B) or lipoprotein (a) [Lp(a)] is not routinely recommended, except in select individuals. If measured, Lp(a) levels >50 mg/dL and apo B ≥130 mg/dL are considered an ASCVD risk enhancer according to the 2018 AHA/ACC cholesterol guidelines.2
References
- Welsh C, Celis-Morales CA, Brown R, et al. Comparison of conventional lipoprotein tests and apolipoproteins in the prediction of cardiovascular disease. Circulation 2019; 140 (7): 542-552.
- Grundy S, Stone N, Beam C, Birtcher KK, Harm PD. 2018 AHA/ACC/AACVPR/AAPA/ ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol. J Am Coll Cardiol 2019; 73 (24): e285-e350.
- Simes RJ, Marschner IC, Hunt D, et al. Relationship between lipid levels and clinical outcomes in the Long-term Intervention with Pravastatin in Ischemic Disease (LIPID) Trial: to what extent is the reduction in coronary events with pravastatin explained by on-study lipid levels? Circulation 2002; 105 (10): 1162-1169.
- Kannel WB, Castelli WP, Gordon T, McNamara PM. Serum cholesterol, lipoproteins, and the risk of coronary heart disease. The Framingham study. Ann Intern Med 1971; 74 (1): 1-12.
- Stamler J, Wentworth D, Neaton JD. Is relationship between serum cholesterol and risk of premature death from coronary heart disease continuous and graded? Findings in 356,222 primary screenees of the Multiple Risk Factor Intervention Trial (MRFIT). JAMA 1986; 256 (20): 2823-2828.
- Ingelsson E, Schaefer EJ, Contois JH, et al. Clinical utility of different lipid measures for prediction of coronary heart disease in men and women. JAMA 2007; 298 (7): 776-785.
- Miller M, Stone NJ, Ballantyne C, et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation 2011; 123 (20): 2292-2333.