Blood glucose levels vary throughout the day based on dietary intake and level of activity as well as based on diabetes and pregnancy status.1-3 For those aged 65 or older, comorbid conditions and overall health also affect recommended blood glucose levels.4 Below is a table outlining American Diabetes Association (ADA) recommendations.
Table 1. Glycemic recommendations based on diabetes status, pregnancy status, overall health in older adults, and method of testing.2-7
|
|
Hemoglobin A1C
|
Fasting plasma glucose
|
Postprandial plasma glucose
|
|
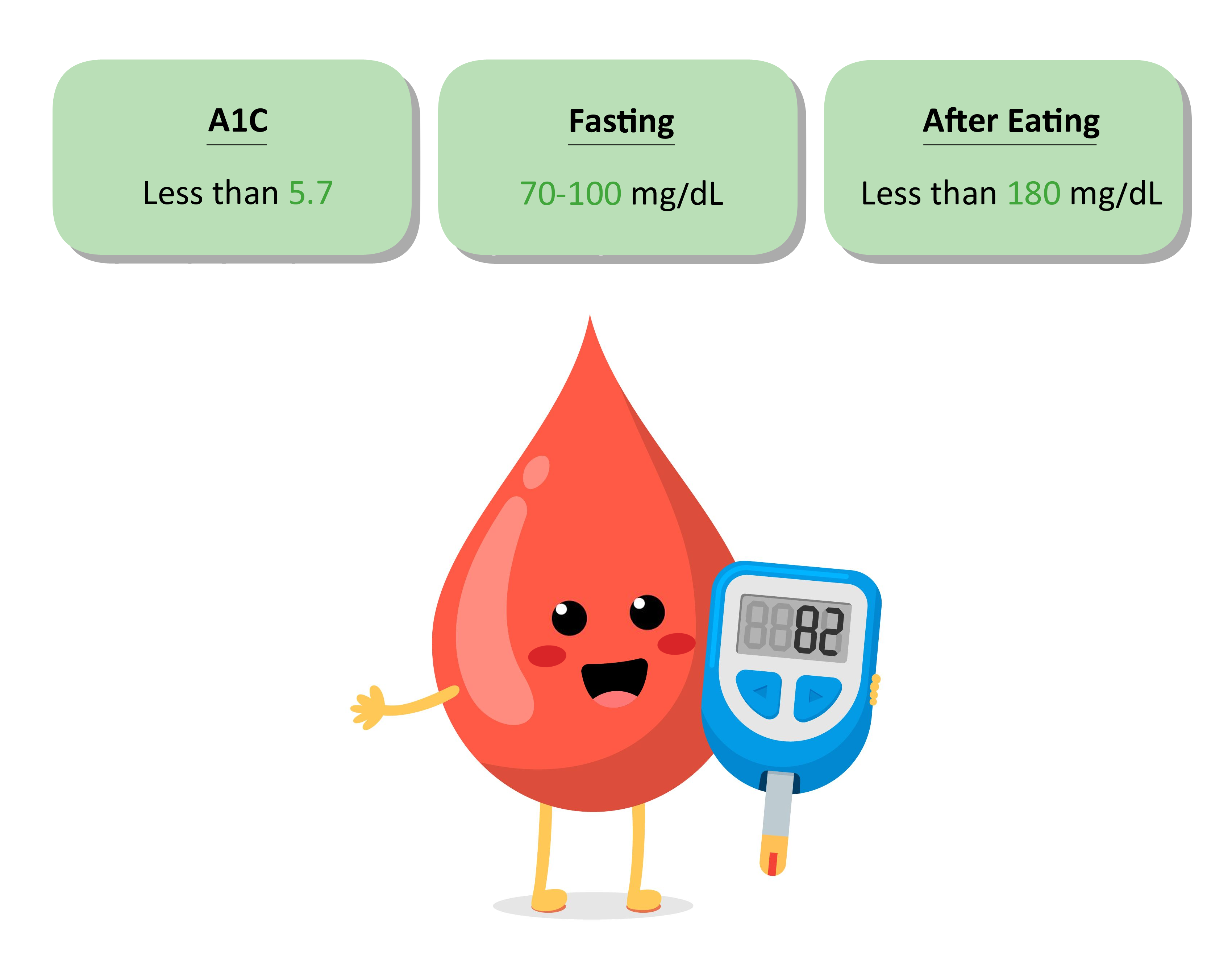
Nondiabetic people of all ages
|
<5.7%
(39 mmol/mol)
|
70-100 mg/dL
(0.6-5.5 mmol/L)
|
<140 mg/dL
(7.8 mmol/L)
|
|
Diabetic, nonpregnant child, adolescent, or adult
|
<7.0%
(53 mmol/mol)
|
80-130 mg/dL
(4.4-7.2 mmol/L)
|
<180 mg/dL
(10.0 mmol/L)
|
|
Diabetic pregnant people of all ages
|
<6.0%
(42 mmol/mol)
|
70-95 mg/dL
(3.9-5.3 mmol/L)
|
100-120 mg/dL
(5.6-6.7 mmol/L)*
|
|
Diabetic older adult in otherwise good health
|
<7.0-7.5%
(53-58 mmol/mol)
|
80-130 mg/dL
(4.4-7.2 mmol/L)
|
N/A
|
|
Diabetic older adult in intermediate health
|
<8.0%
(64 mmol/mol)
|
90-150 mg/dL
(5.0-8.3 mmol/L)
|
N/A
|
|
Diabetic older adult in poor health
|
N/A
|
100-180 mg/dL
(5.6-10.0 mmol/L)
|
N/A
|
*2 hours postprandial plasma glucose
Fasting glucose is measured after a fast of at least eight hours with a baseline blood glucose level being measured in the absence of food intake.2 Postprandial plasma glucose is taken 1-2 hours after the beginning of a meal.
Hypoglycemia is mostly benign in nondiabetic patients, although it can cause uncomfortable symptoms such as shakiness, irritability, confusion, tachycardia, sweating, and hunger.2 Hypoglycemia does have the potential to cause acute harm, especially in older adults and those with uncontrolled diabetes, as it can cause falls, motor vehicle accidents, or other injury. In those with diabetes, hypoglycemia can progress to loss of consciousness, seizure, coma, or death.
Hyperglycemia is associated with increased risk of a variety of health conditions. For nondiabetic patients, persistent hyperglycemia can lead to insulin resistance and the development of type 2 diabetes.8 For diabetic patients, hyperglycemia can lead to the development of atherosclerotic cardiovascular disease (ASCVD), kidney disease, retinopathy, neuropathy, and foot ulceration.9-11
References
- 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes-2024. Diabetes Care. Jan 1 2024;47(Suppl 1):S77-s110. doi:10.2337/dc24-S005
- 6. Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes-2024. Diabetes Care. Jan 1 2024;47(Suppl 1):S111-s125. doi:10.2337/dc24-S006
- 15. Management of Diabetes in Pregnancy: Standards of Care in Diabetes-2024. Diabetes Care. Jan 1 2024;47(Suppl 1):S282-s294. doi:10.2337/dc24-S015
- 13. Older Adults: Standards of Care in Diabetes-2024. Diabetes Care. Jan 1 2024;47(Suppl 1):S244-s257. doi:10.2337/dc24-S013
- 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes-2024. Diabetes Care. Jan 1 2024;47(Suppl 1):S20-s42. doi:10.2337/dc24-S002
- Diagnosis TECot, Mellitus CoD. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997;20(7):1183-1197. doi:10.2337/diacare.20.7.1183
- 14. Children and Adolescents: Standards of Care in Diabetes-2024. Diabetes Care. Jan 1 2024;47(Suppl 1):S258-s281. doi:10.2337/dc24-S014
- Jallut D, Golay A, Munger R, et al. Impaired glucose tolerance and diabetes in obesity: a 6-year follow-up study of glucose metabolism. Metabolism. Oct 1990;39(10):1068-75. doi:10.1016/0026-0495(90)90168-c
- 10. Cardiovascular Disease and Risk Management: Standards of Care in Diabetes-2024. Diabetes Care. Jan 1 2024;47(Suppl 1):S179-s218. doi:10.2337/dc24-S010
- 11. Chronic Kidney Disease and Risk Management: Standards of Care in Diabetes-2024. Diabetes Care. Jan 1 2024;47(Suppl 1):S219-s230. doi:10.2337/dc24-S011
- 12. Retinopathy, Neuropathy, and Foot Care: Standards of Care in Diabetes-2024. Diabetes Care. Jan 1 2024;47(Suppl 1):S231-s243. doi:10.2337/dc24-S012