[NOTE: This article has been posted prior to peer review for use in an active research program. This content will be updated with a peer reviewed version as soon as it is available.]
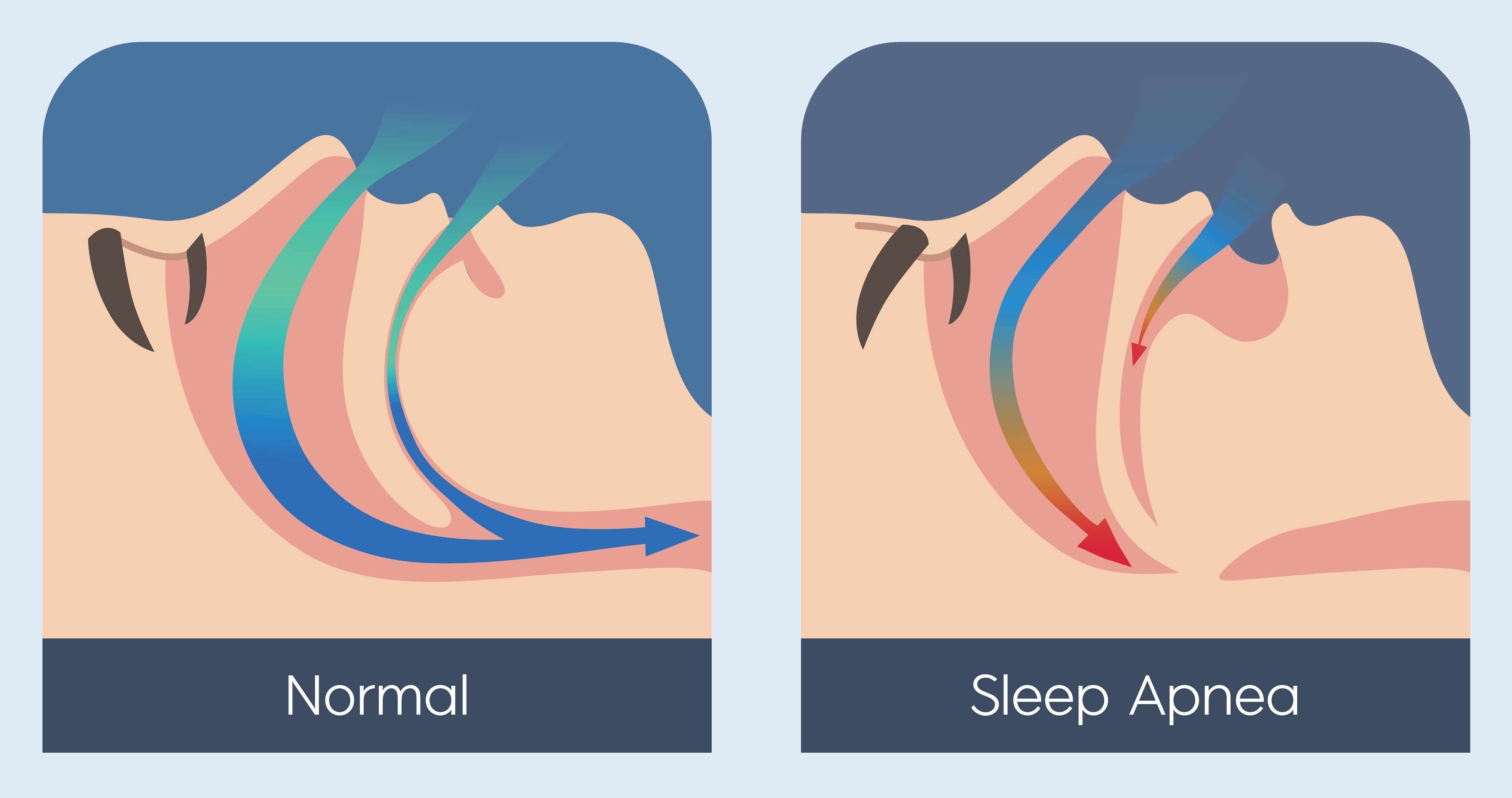
There are four groups of sleep-related breathing disorders as defined by the American Academy of Sleep Medicine’s (AASM) International Classification of Sleep Disorders: obstructive sleep apneas (OSAs), central sleep apnea (CSA) syndromes, sleep-related hypoventilation disorders, and sleep-related hypoxemia disorder.1 Both OSA and CSA are characterized by episodes of narrowing of the upper airway that impairs normal ventilation during sleep.1,2 However, they differ in pathophysiology. OSA is musculoskeletal in nature, with muscle relaxation leading to tissue in the throat impeding the airway.3 CSA is caused by abnormal brain signaling during sleep, although the exact cause of CSA is not well understood.
Both OSA and CSA can lead to hypoxia, hypercapnia, intrathoracic pressure swings, and increased sympathetic nervous activity, all of which disrupts sleep. Symptoms include unrefreshing sleep, daytime sleepiness, fatigue, insomnia, awakening with gasping or choking sensation, and loud snoring.
Obstructive Sleep Apnea
The diagnosis of OSA involves measuring breathing during sleep using polysomnography or home sleep apnea testing.2,4 Several medical conditions are associated with OSA, including hypertension, coronary artery disease, atrial fibrillation, congestive heart failure, stroke, diabetes, cognitive dysfunction, or mood disorder.
The International Classification of Sleep Disorders diagnostic criteria for OSA are:1
- having signs and symptoms or associated medical conditions coupled with ≥5 obstructive respiratory events per hour of sleep;
- or ≥15 obstructive respiratory events per hour even in the absence of symptoms or associated medical conditions.
The first-line treatment for OSA is continuous positive airway pressure (CPAP).5 Mandibular advancement devices can also be appropriate for mild to moderate OSA. If these therapies are ineffective, surgical referral may be helpful, especially in cases where nasal obstruction reduces CPAP adherence or where hypoglossal nerve stimulation therapy or maxillomandibular advancement surgery may be helpful.
Central Sleep Apnea
The International Classification of Sleep Disorders defines eight CSA syndromes: CSA with Cheyne-Stokes breathing, CSA due to a medical disorder without Cheyne-Stokes breathing, CSA due to high altitude periodic breathing, CSA due to a medication or substance, primary CSA, primary CSA of infancy, primary CSA of prematurity, and treatment-emergent CSA.1
The diagnosis of CSA also involves measuring breathing during sleep using polysomnography or home sleep apnea testing.4 The subtypes of CSA have differing diagnostic criteria; however, all require having signs and symptoms, ≥5 obstructive respiratory events per hour of sleep, and the disorder not being better explained by another current sleep disorder, medical disorder, medication, or substance use.1
Diagnostic criteria for specific subtypes also include the following:1
- CSA with Cheyne-Stokes breathing – evidence of Cheyne-Stokes breathing
- CSA due to a medical disorder without Cheyne-Stokes breathing – presence of a medical disorder associated with sleep apnea and no evidence of Cheyne-Stokes breathing
- CSA due to high altitude periodic breathing – occurs at high altitude
- CSA due to a medication or substance – patient is taking an opioid, ticagrelor, or other medication known to impact respiratory control
- Primary CSA – no evidence of Cheyne-Stokes breathing and no evidence of daytime or nocturnal hypoventilation
- Primary CSA of infancy – no evidence of Cheyne-Stokes breathing, no evidence of daytime or nocturnal hypoventilation, and occurs during infancy
- Primary CSA of prematurity – no evidence of Cheyne-Stokes breathing, no evidence of daytime or nocturnal hypoventilation, and occurs in children
- Treatment-emergent CSA – occurs during treatment for OSA
The first-line treatment for is CPAP primary CSA, CSA due to heart failure, CSA due to medication or substance use, treatment-emergent CSA, and CSA due to a medical disorder.6 Bilevel positive airway pressure (BPAP) with a backup rate, adaptive servo ventilation (ASV), or oral acetazolamide can also be used for these conditions, although evidence of their effectiveness is less conclusive. The use of BPAP without a backup rate is not recommended. AASM also recommends using low-flow oxygen in patients with CSA due to heart failure and CSA due to high altitude. Acetazolamide can also be used for patients with CSA due to high altitude. While transvenous phrenic nerve stimulation (TPNS) may be used for primary CSA and CSA due to heart failure, it is both an invasive procedure and not universally available, so AASM recommends considering other treatment options first.
Cardiovascular Disease Risk
There is an association between disordered sleep, especially sleep apnea, and cardiovascular health, but the exact relationship is not completely understood.7-9 While sleep apnea has been shown to affect risk for a variety of cardiovascular conditions (e.g., hypertension, atrial fibrillation, stroke) and aspects of cardiovascular function (e.g., intrathoracic pressure and abnormalities of cardiovascular autonomic regulation),10,11 there have been studies with modest or mixed findings for other cardiovascular conditions (e.g., ischemic heart disease).12 Due to comorbidities and confounding factors such as the prevalence of obesity among those with sleep apnea, it can be difficult to ascertain whether any direct impacts on cardiovascular disease risk or progression. There are also limited data regarding the efficacy of treatment reducing risk. Even so, emerging evidence points to a causal relationship between sleep apnea and cardiovascular disease.
OSA has been causally linked to hypertension, with one cohort study published in 2000 (n=709) finding that the presence of hypertension after four years was dependent on the severity of OSA at baseline.13 Among those with a baseline apnea-hypopnea index (AHI) of 0 at baseline, the incidence of stage 2 hypertension rose from 7% at baseline to 10% after four years. Among those with a baseline AHI of 0.1-4.9, stage 2 hypertension rose from 10% to 17%; for AHI 5.0-14.0, hypertension rose from 23% to 28%; and for AHI ≥15, hypertension rose from 36% to 49%. Adjusting for baseline hypertension status, non-modifiable risk factors, body mass index, waist circumference, neck circumference, and weekly alcohol and cigarette use, hypertension was still linked to baseline AHI scores (Odds Ratio [OR] 1.42 for AHI 0.1-4.9, OR 2.03 for AHI 5.0-14.9, and OR 2.89 for AHI ≥15; p=0.002).
Similarly, a 2005 case-control analysis of the Sleep heart Health Study (n=566) found that participants with sleep apnea were more likely to have atrial fibrillation (4.8% vs 0.9%, p=0.003), non-sustained ventricular tachycardia (5.3% vs 1.2%, p=0.004), and complex ventricular ectopy (25.0% vs 14.5%, p=0.002).14 After adjusting for age, sex, body mass index, and prevalent coronary heart disease, those with sleep apnea were still more likely to have atrial fibrillation (OR 4.02), non-sustained ventricular tachycardia (OR 3.40), and complex ventricular ectopy (OR 1.74).
A 2005 observational cohort study (n=1,022) found that over six years of follow-up participants with higher AHI were more likely to suffer a stroke.15 The incidence of stroke was 3.16% among those with OSA compared to 0.62% among the control group with an AHI ≤3.
While there is strong evidence that OSA is causally linked to several aspects of cardiovascular health, some studies seeking to establish a similar relationship with other forms of cardiovascular disease have had contradictory findings. For example, a 2014 meta-analysis of six cohort studies found no significant association between OSA and ischemic heart disease.16 Similarly, there have been conflicting findings regarding OSA’s relationship to acute coronary syndrome.17 Studies examining the relationship between heart failure and sleep apnea have also had mixed results, with findings from the 2010 Sleep Heart Health Study finding that there was a relationship for women but not for men.18
While these specific conditions and treatment effects on cardiovascular risk require further study, there is a definitive link between sleep apnea and cardiovascular health. The American Heart Association recommends that patients with poorly controlled hypertension, pulmonary hypertension, and recurrent atrial fibrillation be screened for OSA.7 They further recommend that patients with OSA be treated, including behavioral modifications and weight loss as indicated.
References
- International Classification of Sleep Disorders. 3rd ed. Darien, IL: The American Academy of Sleep Medicine; 2014.
- Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. Mar 15 2017;13(3):479-504. doi:10.5664/jcsm.6506
- Rowley JA, Badr MS. Anatomy and Physiology of Upper Airway Obstruction. Principles and Practice of Sleep Medicine. 7th ed. Elsevier; 2022:1170-1183.e6:chap 126.
- Troester M, Quan S, Berry R, et al. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Version 3. Darien, IL: American Academy of Sleep Medicine; 2023.
- Drowos J. Obstructive Sleep Apnea and Chronic Insomnia Disorder: Updated Guidelines from the VA/DoD. Am Fam Physician. Apr 1 2021;103(7):442-443.
- Badr MS, Khayat RN, Allam JS, et al. Treatment of central sleep apnea in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. Aug 18 2025;doi:10.5664/jcsm.11858
- Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/american College Of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation. Sep 2 2008;118(10):1080-111. doi:10.1161/circulationaha.107.189375
- Parati G, Lombardi C, Narkiewicz K. Sleep apnea: epidemiology, pathophysiology, and relation to cardiovascular risk. Am J Physiol Regul Integr Comp Physiol. Oct 2007;293(4):R1671-83. doi:10.1152/ajpregu.00400.2007
- Wright J, Johns R, Watt I, Melville A, Sheldon T. Health effects of obstructive sleep apnoea and the effectiveness of continuous positive airways pressure: a systematic review of the research evidence. BMJ (Clinical research ed). Mar 22 1997;314(7084):851-60. doi:10.1136/bmj.314.7084.851
- Leung RS, Bradley TD. Sleep apnea and cardiovascular disease. Am J Respir Crit Care Med. Dec 15 2001;164(12):2147-65. doi:10.1164/ajrccm.164.12.2107045
- Kasai T, Floras JS, Bradley TD. Sleep apnea and cardiovascular disease: a bidirectional relationship. Circulation. Sep 18 2012;126(12):1495-510. doi:10.1161/circulationaha.111.070813
- Golbin JM, Somers VK, Caples SM. Obstructive sleep apnea, cardiovascular disease, and pulmonary hypertension. Proc Am Thorac Soc. Feb 15 2008;5(2):200-6. doi:10.1513/pats.200708-143MG
- Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. May 11 2000;342(19):1378-84. doi:10.1056/nejm200005113421901
- Mehra R, Benjamin EJ, Shahar E, et al. Association of nocturnal arrhythmias with sleep-disordered breathing: The Sleep Heart Health Study. Am J Respir Crit Care Med. Apr 15 2006;173(8):910-6. doi:10.1164/rccm.200509-1442OC
- Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. Nov 10 2005;353(19):2034-41. doi:10.1056/NEJMoa043104
- Xie W, Zheng F, Song X. Obstructive sleep apnea and serious adverse outcomes in patients with cardiovascular or cerebrovascular disease: a PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore). Dec 2014;93(29):e336. doi:10.1097/md.0000000000000336
- Bauters F, Rietzschel ER, Hertegonne KB, Chirinos JA. The Link Between Obstructive Sleep Apnea and Cardiovascular Disease. Curr Atheroscler Rep. Jan 2016;18(1):1. doi:10.1007/s11883-015-0556-z
- Gottlieb DJ, Yenokyan G, Newman AB, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. Jul 27 2010;122(4):352-60. doi:10.1161/circulationaha.109.901801